Acanthamoeba Keratitis (also known as AK) is a very painful eye condition affecting the cornea. Although it's a rare infection, it is more common amongst contact lens users. Anyone with a corneal injury is also susceptible to developing the infection. It can have severe complications for sufferers, resulting in visual impairments or permanent vision loss. A corneal transplant is necessary in severe cases.
Acanthamoeba Keratitis is challenging to diagnose and difficult to treat. By following a careful contact lens wear routine, you can reduce the risk of infection with Acanthamoeba. You should take care when inserting and removing lenses. An excellent eye care regime can also reduce the likelihood of getting Acanthamoeba Keratitis.
What are Acanthamoeba?
Acanthamoeba is naturally occurring, free-living amoeba (one-celled organisms). Acanthamoeba lives in sources such as tap water, sewer systems, soil, swimming pools, hot tubs and saunas. When we encounter Acanthamoeba, in general, it doesn't cause any harm; however, when amoeba infects the cornea, this results in Acanthamoeba Keratitis.
How do you get Acanthamoeba Keratitis?
You can get Acanthamoeba Keratitis if contaminated water comes into contact with the eye. The following increases the risk of getting acanthamoeba keratitis:
- Wearing contacts in the shower
- Wearing contact lenses while swimming
- Using non-medical approved contact lens solutions
- Storing your lenses in water
- Failing to wash your hands thoroughly before handling contact lenses
- Using an old solution
- Failing to disinfect your lenses effectively
- Following an inadequate cleaning regime
It would help if you avoided these risk factors at all costs.
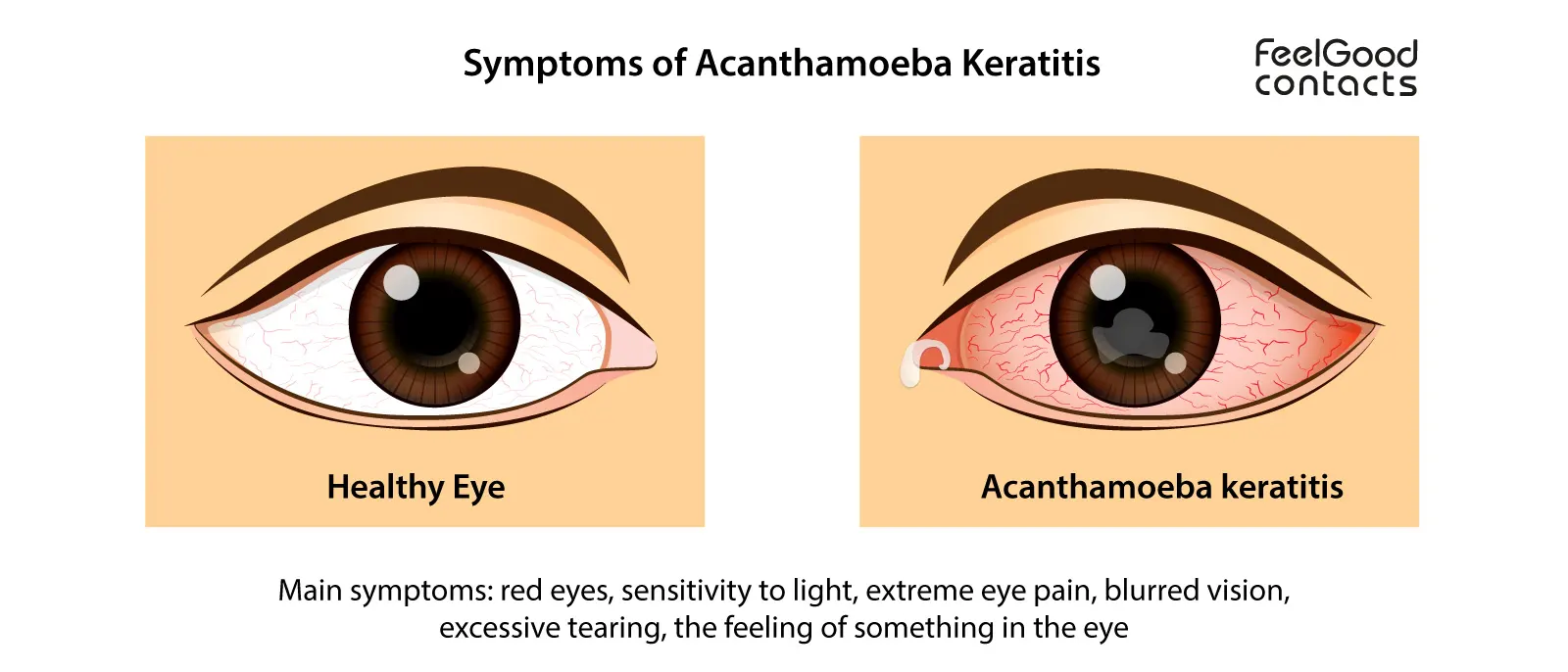
What are the symptoms of Acanthamoeba Keratitis?
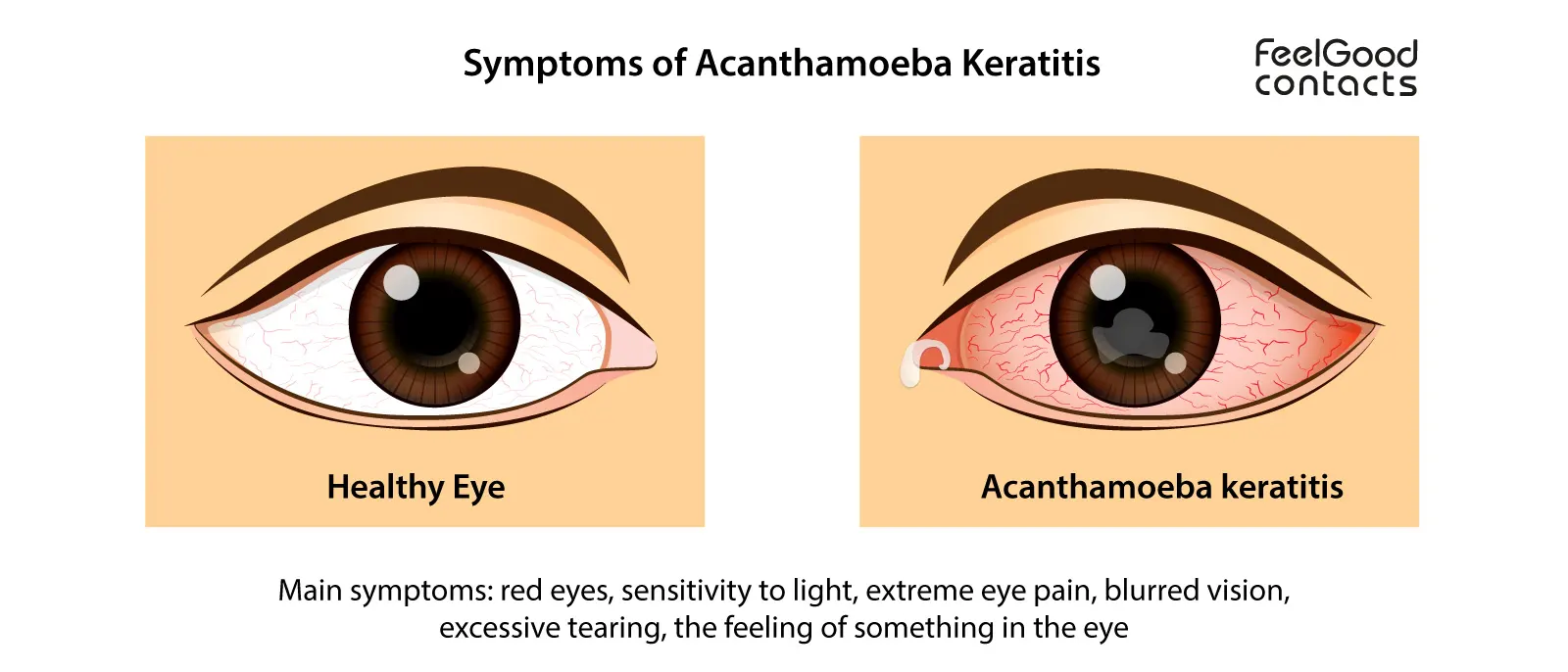
Acanthamoeba Keratitis can be difficult to initially detect as the symptoms are very similar to other common eye infections. Some of these symptoms include:
- Red eyes
- Increased sensitivity to light
- Extreme eye pain
- Blurred vision
- The constant feeling of something in the eye
- Excessive tearing
Infected eyes can often display a white ring around the iris and severe redness. A ring-shaped ulcer can also appear in later phases of the infection.
If you experience any of these symptoms, remove your contact lenses and consult your contact lens practitioner/optician immediately, who will advise you what to do next.
How do you diagnose Acanthamoeba Keratitis?
Your ophthalmologist will perform a range of tests to diagnose Acanthamoeba Keratitis. They will look for inflammation to your cornea and clinical signs of Acanthamoeba Keratitis using a slit lamp microscope.
A corneal scrape and culture sometimes follow the slit lamp microscope test. In this procedure, cells from the cornea are examined in a laboratory.
Alternatively, a test called PCR is used on a swab of the cornea to check for the Acanthamoeba DNA.
In some cases, confocal microscopy can diagnose Acanthamoeba Keratitis. Confocal microscopy involves a powerful scanner that can detect Acanthamoeba cysts within the layers of the cornea.
Acanthamoeba Keratitis is similar to other microbial corneal infections in the early stages so it may be difficult to tell them apart initially. Therefore, it is important to do a variety of tests and observe clinical signs and symptoms.
Sometimes a diagnosis is changed based on the way your eyes respond to treatment or once more information from the lab tests have been received.
How can I prevent Acanthamoeba Keratitis?
You can prevent Acanthamoeba Keratitis by practising good hygiene and an effective lens care routine while wearing contact lenses.
We suggest reading our page on how to correctly insert and remove your contact lenses. It is also important to listen carefully to the advice of your contact lens practitioner/optician and always follow their instructions on lens wear and care.
In summary, here are the main actions you can take to avoid infection with soft contact lenses:
- Wash your hands thoroughly with mild soap and water. Dry your hands with a lint-free towel before handling contact lenses
- Only use the lens care system which has been recommended to you by your optician and do not mix with other solutions
- Also, note the different purposes for different solutions. Saline solution, for example, is not appropriate for disinfecting, and can only be used for wetting and short-term storing
- Use fresh solution each time you clean your lenses and contact lens case
- Don't sleep in lenses unless they are extended wear lenses, prescribed to you by your optician
- Don’t wet contact lenses with water or saliva
- Never use lenses that were worn by someone else
- Gently rub and rinse contact lenses before inserting and after removing them, before putting them back into their case
- Replace your lens case every three months
- Avoid swimming with contact lenses
Is Acanthamoeba Keratitis treatable?
Acanthamoeba is much more challenging to treat than other microbial infections. Antibiotics cannot treat Acanthamoeba.
There are no medical treatments for Acanthamoeba Keratitis. Procedures are mostly done by trial and error depending on what the patient responds too. For this reason, an early diagnosis is incredibly important.
One method of treatment is a high dosage of topical antimicrobial agents on the area of the infection site. Cysts can become highly resistant to therapy, so a potent combination of substances is required.
A recommended combination may include chlorohexidine (0.02%) and polyhexamethylene biguanide (PHMB, 0.02%) for treating both the trophozoites and cysts. Using one of these agents in combination with propamidine (Brolene) or hexamidine (Desmodine) may also be suggested.
In addition to this, a prescription of anti-inflammatories can relieve the pain. A dilating drop used early on in the infection can prevent painful spasms of the eyelid.
How long does Acanthamoeba Keratitis last?
The length of time at which Acanthamoeba Keratitis persists when undergoing treatment is not known. The duration of the infection may differ depending on its severity and the methods being used to treat it. According to the BCLA, if AK is recognised later then intensive treatment may be needed for up to 12 months. Infection can also reoccur after treatment.
When to see a doctor
You should see an eye care professional or optician immediately if you experience any symptoms of Acanthamoeba Keratitis. Depending on the severity of the symptoms, they may refer you to an ophthalmologist.
An early diagnosis is essential for your eye care professional or optician to provide you with effective treatment. Make sure you prepare for your appointment by writing down a list of questions to ask your eye care practitioner/optician and making a list of any medications that you're currently taking. If you've been swimming with contact lenses, make sure to mention this too.
Quick links:
Can I swim with contact lenses?
Can I clean my contact lenses in water?
A guide to eye infections
Disclaimer: The advice in this article is for informational purposes only and does not replace medical care or an in-person check-up. Please check with an eyecare professional before purchasing any products or remedies. For information on our article review process, please refer to our Editorial Policy.

 Offers
Offers Account
Account
 Favorite
Favorite
 Basket
Basket

 OFFERS
OFFERS